On 30th April 2014 I had the pleasure of being invited to the second stakeholders meeting of the Nuffield Council on Bioethics. It was a pleasure to be invited once again to participate in this workshop/ meeting. The meeting was a fantastic chance to catch up on the progress of the working party group, help feed into their work more as well as a chance to meet more young people and hear their views, thoughts and experiences of research. Furthermore, on a personal note to get to learn more about Medical research involving children and young people, as well as the complex questions and situations which researchers have to deal with. Having been involved in clinical research at a young age and actively trying to get greater involvement of children and young people in research, this project gave me a fantastic opportunity to learn more about how research was conducted in the UK, especially in regards to children and young people. I had the pleasure of attending the very first stakeholders group meeting in July 2013 with several of my RCPCH YAP buddies, and you can read more about our thoughts and experiences from the day on the guest blog post that alongside Ravi and I wrote for the Nuffield Bioethics Blog: http://blog.nuffieldbioethics.org/?p=811 In this post, I hope to highlight some of the key thoughts alongside some of my reflections from the day, with a particular focus of new clinical trials and the role of ethics committees, the topic of 'vulnerability' of children and young people and also the issue of decision making, consent and assent, which seems always to be a contentious point of discussion. The three points which I am highlighting in this blog were the three big questions identified by the working party. Clinical Trials and Ethic CommitteesIn my opinion, this was the most interesting and appealing session to me personally. While speaking a lot about my experiences of clinical trials, I never really knew the 'behind the scenes' of clinical research trials and what challenges researchers had to go through before they got to administering the trial. To be honest, I don't think a lot of young people who take part in clinical trials are fully aware of the high level of scrutiny which clinical trials undergo before they get to the young people. Below you can watch the two films we were shown at the workshop, the first one shows a mock up clinical ethics meeting and the second showcases what children and young people thought it was to be a part of clinical trials and what they thought the researcher in the first video could have done better. I think what became the most obvious is the intense scrutiny under which clinical research trials go under before they go 'live'. I think that is something which is very relieving to me, especially when that scrutiny highlights the importance of having the voice of children and young people in research. While it was good to know that the people on the ethics panel were highlighting and raising the concerns of children and young people, the general feeling from the day was that people, especially the children and young people thought that there should be a young person on the panel. More pertinently that the young person on the panel should be someone who has that condition as they are more likely to consider the effects of the research on all aspects of their life and may possibly think of things which the adults may not think of. Further during discussion the researchers need to acknowledge that children and young people have a voice was raised, and that researchers need to be aware that when it comes to young people, it is more about the ability of the young person to make a decision rather than their age. When it comes to children and young people with a long term condition, especially, they are forced to grow up rather quickly, regardless of their age. That was certainly what I found in my personal case, when I got diagnosed, I had to grow up and mature rather quickly. Particularly in my situation, the responsibility to make the decision was a lot more on my hands than in most cases with other children. My parents are not native English speakers, originally from Sri Lanka, the never learnt English, and as a result they never knew the full working of the English Healthcare System as well being new to the condition that I had been diagnosed with. Therefore, I was allowed to make a lot of decisions about my care and therefore, I felt it was more important that the information which was being passed on was more child friendly and accessible to my age. This would link a bit with vulnerability which I will cover later on. Another important discussion point which came as a result of watching these films was the lack of awareness of research in school and in children and young people. Hearing from the other young people present on the day it became apparent that young people were not really aware of research, especially clinical research, unless they were directly involved with research. The children and young people who were aware of research were the 'lucky' individuals who had the chance to be involved in the review process for medical trials such as the Medicines for Children Research Network or people who were involved with the research as participants. This should not be the case, children and young people should all be aware of the benefits of clinical research and the steps involved with it. More discussions, like the one illustrated in the second video should be held in schools and create active discussion about research. This would help to alleviate the generally negative image that is associated with research. For example, if researchers were willing and able to go into schools and actively participate in these discussions, by going into schools and leading these workshops it would not only boost children and young peoples knowledge and engagement with clinical research, it would also give researchers a chance to advertise and promote their work in a positive light, as it was intended. Often the portrayal of clinical research can be skewed by the media, and it would be useful and enlightening for children and young people to hear about these trials and benefits of such research from the "horses mouth", as it were. In my experience, I never got taught about clinical trials and research in school, my only knowledge came from my previous involvement in them. I feel my peers would have looked on clinical research with more of a positive light if we openly discussed it in science classes or during PHSCE lessons. Those were the three major points which I would pick out from the discussions which arose from watching the video, however, there were more general points that researchers should pay attention to when coming up with research proposals and while they are conducting their research:
You can find more recommendations that I made, in relation to this, from the 'Turning the Tide' launch here.
Vulnerability The topic of this discussion focussed on whether or not children were vulnerable in research? The dictionary definition of vulnerability is when an individual is "capable of being physically or emotionally wounded or hurt". In order to "protect" individuals who are considered to be "vulnerable", the government puts in place laws in order to protect them. Obviously it is our duty to ensure that the vulnerable are protected, that is one of the reasons why there was such an uproar against the actions of Mid - Staffordshire, amongst other things. When you are in hospital, that is when you are at your most vulnerable and you expect the best standard of care while you are there. The high levels of poor care combined with the high mortality rates that was witnessed at Mid - Staffordshire is not acceptable. This is one of the reasons why looking at vulnerability is important. To ensure, people who need care do not slip through the net and to ensure they are being looked after and cared for properly. As a way of protecting children and young people, who are considered to be vulnerable, the question is raised over whether children and young people need protecting from the responsibility of decision making - or if they need to be involved in making joint decisions as they get older. However, in my opinion sometimes the age restrictions that go along with these laws which define when someone can do something is a bit unfair. This is especially true when it comes to medical care. Sometimes while a young person maybe under- age in the eyes of the law in order to make a decision, they maybe very mentally capable and more mature then they are in actual age. To this end, young people are more vulnerable when it comes to being involved in decisions is that they don't have appropriate access to information and the lines of communication between the young person and the medical team may be inappropriate for the age of the young person. Ways of combating vulnerability:
To summarise, I would say that vulnerability as a concept cannot and should not be fully disregarded. It is a very important aspect of care and should be upheld as a concept to protect those who need it, for example young babies, people with certain mental health difficulties, etc. However, I feel that we can start reducing the amount of vulnerability that individual face by first reducing and dealing with the risks that can cause vulnerability by involving parents, carers and young people in planning their care, ensuring they all have equal and full information so they are fully equipped to make the right decision and not the decision that is said to be right. To aid in this the use of modern applications and a third party service could be utilised in this process. Further also by ensuring that power relations don't influence decisions of individuals too much. Consent Vs Assent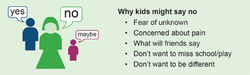 The last part of the day concentrated on a very important issues, that of decision making and assent. This is a topic which gets a lot of discussion going at the RCPCH Youth Advisory Panel meetings. However, due to other commitments I was unable to stay for this portion of the day. However. the inconsistencies in the law which were highlighted in the previous presentation, which made me think a lot. For example. in the UK as soon as you are ten are held responsible for your actions and if you were to commit a crime, then you can be taken to court and locked away. If you can have criminal responsibility at the age of ten, it seems rather strange that you can't refuse consent to procedures outright until you are 18 years old. This made me want to go and do some research into the matter to clarify things for myself. Consent procedures are the most tricky in England and differ from other nations within the UK. For example, in Scotland, parents cannot authorise treatment that a competent young person has refused. This issue seems to be rather an ethical minefield for healthcare professionals, parents/ carers and for children and young people, as such, I am going to deviate a little bit from the discussion of the day to talk about consent and assent, to clarify what they are and my views on this. To start, assent, assent or affirmative consent is defined as the child or young persons' permission or affirmative agreement to participate in research (Broome & Richard, 1998), unlike consent, assent is not mandatory to be obtained. Assent is an opportunity to give children and young people a chance to express their opinions and concerns surrounding participating in research, providing us with a formal means to be included. Assent can also sometimes refers a situation where child understand some but not all the main points required to provide fully informed consent. Sometimes assent can be taken as 'at least not refusing'. While assent is a good way to start conversations about a young persons involvement in their own healthcare, consent is something which takes a greater priority as that is when a young persons decision can really start to impact on their treatment and care. The official Dept. of Health definition of when a person is able to give valid and informed consent is as below: The Department of Health (DH) (2001a) states that when deciding whether a person is This combined with another term which is often thrown around, Gillick competency, makes the foundation of when a child can give consent. Gillick competency refers to English medical law, which is used to decide whether a child (16 years or younger) is able to consent to his/her own medical treatment, without the need for parental permission. So while you can give consent to go ahead with treatment while you are still a (competent) child, the issue of refusing treatment, in essence refusing to consent, even though your parents want you to go ahead with the treatment is another tricky area which I discovered. In this situation, according to the sources I referred to, healthcare professionals can legally overrule the decision of the child and go ahead with the treatment if the parent has given consent. This is something which confuses me and would be something that I would need more clarification and research on, but my initial thoughts would be, if as I mentioned before you can take criminal responsibility at age 10, why can you not be allowed to take decisions about your life and health if you are older than 10 but younger than 18? It seems an absurd concept to me that you can take decisions to accept healthcare if you are deemed to be competent against parents wishes but you aren't allowed to refuse treatment based on your own wishes. If you are deemed competent enough to make decisions and consent to procedures, seems a bit weird you don't seem to have the responsibility to do the opposite. Some young people would argue, especially those who were diagnosed with long term conditions, that since diagnosis they grew up quite quickly and learnt to take control of their condition from very young. Therefore, some would argue that at the the end of the day it is 'our bodies, our lives, our rights', therefore, if we are deemed to be responsible enough to give consent in certain situations, why we can't have the right to refuse consent if we were to fully understand the consequences? However, I digress, this is the topic of a much longer, better researched blog post. Returning to the subject of consent in its current state, I wish to share my reflections from the notes from this meeting on how consent should be managed. From discussions of the other young people, it became apparent there were three different levels of perception on how consent should be managed:
I agree with all the three forms of consent procedures which the young people suggested they felt the most comfortable with during this meeting. Obviously, every young person is different and we all have our different preferences and that is something which I and we all have to respect. Ultimately what is important though is that information should be made available in a way that is accessible to children and young people! While doing research for this post, there was not a single document which made it clear the consent/ assent procedures and key definitions in a way that is accessible to children and young people. This needs to change! The information that is available is written in speak that is suitable for clinicians and healthcare professionals, while that is who this information should be aimed at, it is really important that this information is replicated and issued in a way that children and young people can understand. At the end of the day, as I said before, it is 'our bodies, our lives, our rights, and our futures', therefore, we need to be able to understand those things as easily as possible, if we wanted to! ConclusionOverall, this second workshop meeting for this project, for me was certainly very illuminating and thought provoking. It gave me insights into the working of ethic committees and also gave me fruit for thought in regards to the big concepts of vulnerability and on the issues surrounding consent and assent. While, the purpose of the event was to help the work of the Nuffield Bioethics Working Group, it also served as an opportunity to make me think about the ideas and concepts behind the topics which I talk a lot about during my speeches and presentations with my work with the RCPCH. I am really delighted have been offered a chance to be involved in this project and I look forward to future meetings and workshops. You can find out more information about the working group and follow the progress of the project on their website; http://www.nuffieldbioethics.org/children-and-research
2 Comments
14/8/2014 07:53:24 pm
Thank you very much Thines for sharing your reflections on our project and on issues that came up during this meeting. We really value your input! It was a great day with lots of helpful discussion and feedback which gave the Working Party lots to think about as they start writing up their report!
Reply
Leave a Reply. |